[ad_1]
By Matthew A. Michela
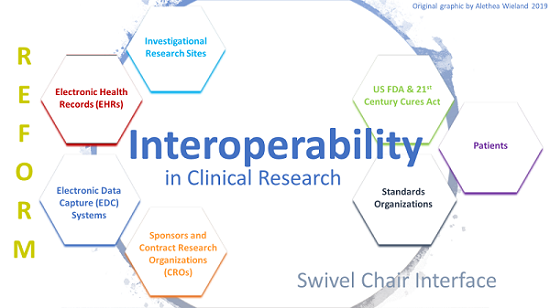
Inadequate access to medical data because of poor interoperability results in suboptimal care and increased costs to both patients and healthcare organizations.
Until recently, interoperability was considered a secondary priority by many health IT companies because of misaligned financial incentives, resistance to change, an overabundance of varied technical standards, and preference for incompatible proprietary technologies.
Today, the 21st Century Cures Act mandates interoperability and electronic access to patient health data. Consider these five tips to help comply with the rules and become a part of advancing patient-centric interoperability:
1. Conduct an Internal Assessment. Take time to understand what the Cures Act aims to accomplish: preventing data blocking and providing patients greater access to clinical data electronically by breaking down data silos and eliminating outdated technology.
Certain clinical data types defined under the United States Core Data for Interoperability (USCDI) set must be available electronically to patients without special effort on their part. Data covered under USCDI will expand over the next few years, covering most essential electronic health data.
2. Adopt Modern Technology. Healthcare is decades behind other industries when it comes to data accessibility. CDs, printers, and fax machines are still in widespread use for sharing information with patients. Though outdated and cumbersome, these technologies are still common because more consideration is often placed on the convenience of maintaining a historical workflow than the long-term benefits of shifting to a digital solution.
The Cures Act includes requirements to adopt technology that uses common industry standards, such as HL7 and FHIR, and application program interfaces (APIs) to create an app economy in healthcare and eliminate challenges patients encounter when manually tracking down and couriering physical copies.
3. Vet Your Vendors. Many healthcare facilities will seek IT solutions to help them achieve true interoperability and rule compliance. When selecting an IT vendor consider the following:
- Ability to handle advanced data: As USCDI expands, unstructured data types such as radiology and pathology will be required as part of electronic health information (EHI). IT solutions should be scalable to incorporate the growing types of clinical data.
- Mature, reputable solutions: Many tech startups tout innovation and disruption, but interoperable technology has existed for 15 years. Mature, experienced vendors can offer a track record on reliability, scalability, and security. Vendors should also provide support services for integration into your enterprise systems.
- “Off the shelf” API tools: These tools enable access to a broad variety of clinical data such as EHR data, labs, and imaging as well as medical networks such as health information exchanges (HIEs) and other data networks that support common standards, such as HL7 and FHIR.
4. Consider Patients. Patients are tech-savvy and are growing frustrated by the barriers and burdens they face trying to manage their health data offline. Like banking or ridesharing, the policy’s goal is to enable patients to open an app and have the medical information they need as they are able to do in nearly every other industry.
As a result, the next generation of patient portals are necessary to share both advanced USCDI data but also grant patient ownership of their health information. Currently, most portals available are limited to viewing access of basic patient information from a single institution or health system. A truly valuable portal offers functionality to not only view but request and store EHI across providers and over time, as well as to share that data bi-directionally between patients and their care teams.
If your portal cannot handle complex data, consider a vendor-agnostic portal or integration solution to enhance your existing portal with access to clinically valuable data from different sources to create a complete history of a patient.
5. Get to the Cloud and Continue to Innovate. Healthcare providers must have as much relevant clinical data in advance as possible to make appropriate care decisions. Much of that data is locked into silos. Through the cloud, providers have access to valuable patient data from numerous sources to enable better care coordination and treatment decisions. The value to this standardized data at the point of care is tremendous but also spurs innovation with access to more diverse sets of data for research teams to advance the understanding of diseases and treatments and AI developers to validate algorithms.
Matthew A. Michela (ceo@lifeimage.com) is president and CEO of Life Image.
Leave a comment
[ad_2]