Trend Toward More Expensive Inpatient Hospital Stays in Medicare Emerged Before COVID-19 and Warrants Further Scrutiny.
Hospitals have long been essential providers in our healthcare system. Medicare payments reflect their importance: nearly one-fifth of all Medicare payments are for inpatient hospitalizations. In fiscal year (FY) 2019—prior to the COVID-19 pandemic—Medicare spent $109.8 billion for 8.7 million inpatient hospital stays. Trends in inpatient hospitalizations from FY 2014 through FY 2019 provide important lessons for improving the accuracy of inpatient hospital billing. From this information, stakeholders can gain a better understanding of how hospitals bill Medicare and of vulnerabilities that Medicare should address. The pandemic has placed unprecedented stress on the country’s health care system, making it more important than ever to ensure that Medicare dollars are spent appropriately.
The COVID-19 pandemic has placed a financial strain on the country’s health care system, making it more important than ever to ensure that Medicare dollars are spent appropriately. Oversight is essential, particularly for inpatient hospital stays, which account for a significant share of Medicare spending.
Inpatient hospital billing in the years leading up to the pandemic indicates that some stays at the highest severity level could be susceptible to inappropriate billing. Accordingly, we recommend that the Centers for Medicare & Medicaid Services (CMS) conduct targeted reviews of MS-DRGs and stays that are vulnerable to upcoding, as well as the hospitals that frequently bill them.
CMS has the RAC (Recovery Audit Contractors) program that conducts MS-DRG validation, upcoding errors, and improper payment rates.
Why, though, are hospitals being subjected to such surveillance?
As the OIG report, itself, points out, about 20 percent of Medicare’s budget reflects payments to hospitals for inpatient services. That’s a huge chunk of change; and, some time ago, the OIG began to notice an uptick in charges to Medicare relative to inpatients, in particular. In response, agency officials decided to undertake a narrowly defined investigative study on the billing practices of hospitals.
Conduct targeted reviews of MS-DRGs and stays that are vulnerable to upcoding, as well as the hospitals that frequently bill for them.
Upcoding occurs when a hospital bills Medicare for codes that are not appropriate for the
beneficiary’s condition. It can take different forms, such as adding or miscoding diagnoses.
Upcoding can result in an MS-DRG that has a higher severity level and therefore a higher
payment. Indications that this may be happening include:
- Stays at the highest severity level that last a shorter amount of time than the mean
length of stay for the given MS-DRG. This may point to the beneficiary’s being less
sick than the coding signifies. - Stays that reach the highest severity level because of just one diagnosis. This could
mean that the stay was assigned an inappropriately high severity level.
Eyeing the Numbers
The OIG’s study involved an analysis of paid Medicare Part A claims for inpatient hospital stays from FY 2014 through FY 2019. The agency was able to identify certain patterns in billing that pertain to severity levels, which are determined by the Medicare Severity Diagnosis Related Group (MS-DRG). Specifically, the study found the following billing trends:
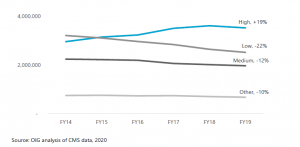
- Hospitals are increasingly billing for inpatient stays at the highest severity level, which is the most expensive one. The number of stays at the highest severity level increased almost 20 percent from FY 2014 through FY 2019, ultimately accounting for nearly half of all Medicare spending on inpatient hospital stays.
- The number of stays billed at each of the other severity levels decreased.
- The average length of stay decreased for stays at the highest severity level, while the average length of all stays remained largely the same.
- Stays at the highest severity level are vulnerable to inappropriate billing practices, such as upcoding—the practice of billing at a level that is higher than warranted.
- Nearly a third of the highest severity level stays lasted a particularly short amount of time, and over half of the stays billed at the highest severity level had only one diagnosis qualifying them for payment at that level.
- Hospitals varied significantly in their billing of these stays, with some billing much differently than most.

Key Takeaways
Hospitals increasingly billed for inpatient stays at the highest severity level—the most
expensive level—from FY 2014 through FY 2019.
There are indications that these stays are vulnerable to inappropriate billing practices, such as upcoding.
U.S. Department of Health and Human Services recommends that CMS conduct targeted reviews of MS-DRGs and stays that are vulnerable to upcoding, as well as the hospitals that frequently bill for them.
For more information review the OIG audit report/CMS audit program for more insight on the audits.
Ref: U.S. Department of Health and Human Services