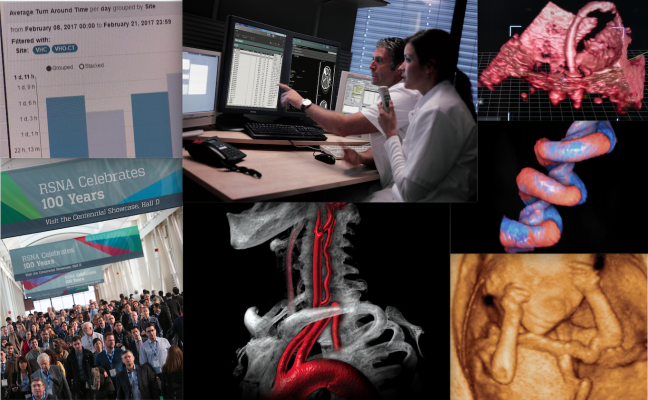
“Radiology is the science that uses medical imaging to diagnose and sometimes also treat diseases within the body.”
- A variety of imaging techniques are used to diagnose/ treat diseases, such as ,
- Computed tomography (CT)
- Ultrasound
- X-ray radiography
- Nuclear medicine including positron emission tomography (PET), and Magnetic resonance imaging (MRI)
Accurate and efficient radiology billing can prove tricky, especially with so many factors influencing the final outcome. Still, maintaining a healthy revenue stream is possible for any healthcare provider so long as the practice adheres to a handful of best practices. Many of them are fairly common sense but, if ignored, can prove detrimental in the long-term.
BEST STRATEGIES: (To get strong results for reimbursement of radiology claims)
Communication:
Coders needs to be confident that they will be able to confirm the necessity of a procedure or the accuracy of the reports they receive prior to billing, in order to avoid costly and time-consuming mistakes so there should be a strong policy of frequent and clear communication between physicians or technicians and coders is critical to ensure the accuracy of radiology billing. It’s always best to catch a mistake prior to a claim being filed, and to decrease the likelihood of a mistake going unnoticed.
Training:
In order to maintain coding credentials coder’s must update their certifications continuously, so is for the billing personnel, they should also be trained with all current billing standards and updates via training sessions.
Educating patients:
Educating patients is also crucial for a healthcare provider. For instance making it clear to the patient that exactly what portion of their testing or procedure will be covered by insurance and also it can be reminding patients upfront that their copay is due at the time of service. Guiding patients in the right direction when it comes to assistance in the often confusing claims and reimbursement processes will also go a long way toward ensuring that bills are settled in a timely and satisfactory manner.
Complete Documentation:
Not only does this include patient information, but it should also include up-to-date records of the state of the patient’s account, so as to avoid confusion in billing and payment.After all, the more accurate the coding, the more quickly a claim can be processed and the higher clean claims rate.
“No documentation equals not done.” Is a golden rule of medical billing and coding .Therefore, a complete radiology report is essential to support proper code assignment and optimal reimbursement, and should include, minimally, the following elements:
- patient name (The ACR Practice Guideline for Communication Of Diagnostic Imaging Findings further encourages documentation of the patient’s date of birth or age and sex);
- referring physician;
- date and time of the study;
- patient history; and
- reason for the study
Practices also must retain the actual radiology images as part of the medical record as well as an order or request for the study And last but not least, providers should encourage communication with coding and billing staff if any information in the report appears to be missing or contradictory to avoid clinical, legal, compliance, and reimbursement problems.