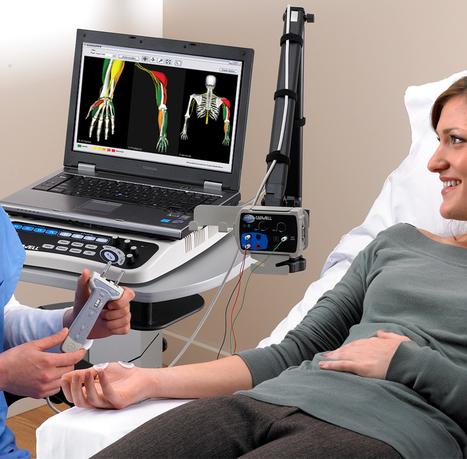
As per AMA, the CPT book Definition of a conduction study is “defined as a sensory conduction test, a motor conduction test with or without an F wave test, or an H-reflex test.
Each type of study, sensory or motor with or without F wave, H-reflex associated with that nerve constitutes a distinct study when determining the number of studies in each grouping, eg. 1-2 or 3-4 nerve conduction studies.” With this coding definition, we can ID
the correct code.
The below Tips are based on most frequent examples of NCV with EMG coding and billing.
Identification of the correct code for NCV studies:
Count the number of motor and/or sensory studies done within each nerve. Example, the Right arms’ median, ulnar, and radial (motor and sensory) nerves are tested. We have 3 nerves with 2 studies in each nerve. This would yield a total of 6 studies (3×2). CPT code is 95909.
Coding for bilateral NCV study:
Using the same example above, I would count each nerve (with study) on both extremities. Motor and Sensory studies in bilateral upper extremities on each three nerves would yield 12 studies; CPT code 95912.
Tip: Look for the terms “motor” and “sensory” (F wave and H-reflex are included and not separately counted). ID the number of nerve(s) tested, then count each motor and sensory test done on each nerve. Don’t forget if it’s done bilaterally to also count that as it can affect the code selection. If it’s a mirror image of the opposite limb, just duplicate that initial limb findings.
Some time we caught with a situation where we think, Can we count the study more than once when performed along the same nerve?
Simply put, NO.
The coding guidelines state “each type of NCV study is counted only once when multiple sites on the same nerve are stimulated or recorded.
Tip: Paraspinal nerves tested within the affected limb are not coded separately as they are included in the NCV code parental description. Paraspinal nerves tested NOT ASSOCIATED with that limb can be separately code (if medical necessity supports) with codes (95860-95864 and 95867-95870).
For example: A neurologist performed a one limb EMG (6 muscles) without any NCV on the same day. Because no NCVs were performed that day on that patient, the old Code 95860 ( Needle Electromyography; 1 extremity with or without related paraspinal areas) should be used.
Identification of the correct code for EMG done with NCV studies:
Use code 95885 when a limited (less than five muscles) are studied within a limb or use code 95886 when a complete (five or more muscles) are studied.
Count the number of muscles for each extremity; if all extremities studied are complete use CPT 95886 once with 4 units.If only two extremities are a complete study and the other two extremities are a limited study, then code 95886×2 units for the complete and 95885×2 units with modifier 59 for the limited.
Tip: Both the printout of the study and the provider’s interpretation with report should mention the number of muscles tested on each limb. The term “all other muscles” without the actual documentation support (either in the printout or report) should not be used to support a higher (95886) code.
Here I am going to summaries my article for easy understanding:
NCV STUDIES:
• 3 Nerves: Median, Ulnar, radial nerves (Studies: Motor and Sensory) ,we have 3 nerves with 2 studies in each nerve this would yield a total of 6 studies (3×2) CPT 95909.
• In case of bilateral studies; I would count in same fashion above, and count it as 12 studies and cpt would be 95912 (note: it’s a mirror image of the opposite limb, just duplicate the initial limb)
• I would not count the study more than once when performed on the same nerve.
• Para spinal nerves tested within the effected limb are not coded separately.
• Para spinal nerves not associated with the limb can be coded separately; with code 95870.
EMG STUDIES:
• Use code 95885 when a limited study performed ( less than 5 muscles)
• Use code 95886 when a complete study performed (five or more muscles)
• Count the number of muscles for each extremity; if all extremities studied are complete use CPT 95886 once with 4 units .
• If only two extremities are complete and two are limited, then use code 95886 x 2 units and 95585 x 2 units..Use 59 modifier for the limited .
Note: The term all other muscles “without the actual documentation support”, should not b used to support a higher code.
Real life example of counting nerve and muscles to code ncv and emg.
For more tips and tricks related to Medical Billing, subscribe my blog newsletter.