Bone mineral density test

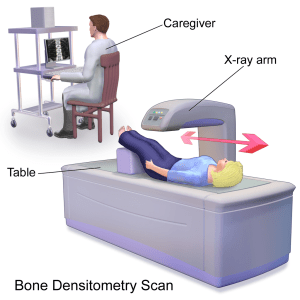
To diagnose osteoporosis before a broken bone occurs, the only test is a bone density test, which can help to estimate the density of your bone. As recommended by National Osteoporosis foundation (NOF) a bone mineral density test of the hip and spin test is being done with central dexa (dual energy x-ray absorptiometry) machine.
Central dexa and peripheral tests are two types of bone density test.
A bone density test of the hip and spine using a central DXA machine to diagnose osteoporosis. When testing can’t be done on the hip and spine, National Osteoporosis foundation (NOF) suggests a central DXA test of the radius bone in the forearm. In some cases, the type of bone density testing equipment used depends on what is available in your community.
For example People of Larger Size. Most central DXA machines cannot measure bone density in the hip and spine of patients who weigh more than 300 pounds. Some newer machines can measure bone density in people who weigh up to 400 pounds, but these machines are not widely available. When the hip and spine cannot be measured, some healthcare providers recommend a central DXA test of the radius bone in the forearm and a peripheral bone density test of the heel or another bone.
Peripheral tests:
• pDXA (peripheral dual energy x-ray absorptiometry)
• pQCT (peripheral quantitative computed tomography)
• QUS (quantitative ultrasound)
These tests are very useful when central dexa is not available and also used to identify people who are more likely to get benefit from further bone density tests.
This test can be in-house from a healthcare provider or patient will be referred to a testing center. People taking an osteoporosis medicine should repeat their bone density test by central DXA every one to two years. After starting a new osteoporosis medicine, many healthcare providers will repeat a bone density test after one year.
T-score is used to determine whether a patient’s bone density is higher or lower than a standard bone density or 30 year old adult. To diagnose osteoporosis a provider looks at the lowest T-score.
• Normal -Bone density is within 1 SD (+1 or −1) of the young adult mean.
• Low bone mass- Bone density is between 1 and 2.5 SD below the young adult mean (−1 to −2.5 SD).
• Osteoporosis- Bone density is 2.5 SD or more below the young adult mean (−2.5 SD or lower).
• Severe (established) osteoporosis- Bone density is more than 2.5 SD below the young adult mean, and there have been one or more osteoporotic fractures.
The age-matched reading, known as the Z-score, compares a person’s bone density to what is expected in someone of equivalent age, sex, and size. However, among older and elderly adults, low bone mineral density is common, so comparison with age-matched norms can be misleading.
In addition to calculating Z-scores and T-scores, the DXA report may include a FRAX (fracture risk assessment tool) score. FRAX uses the bone density measurement, and other risk factors, to calculate a person’s risk of breaking any major bone or hip due to osteoporosis in the next 10 years. FRAX is used for those people who have not yet taken bone-building medication. If the probability of a hip fracture in the next 10 years is calculated to be more than 3%, or the probability of a fracture of any major bone due to osteoporosis is greater than 20%.
For more updates to related medical documentation, follow me and signup my newsletter.